Back
Diabetes and the Cardiometabolic Continuum
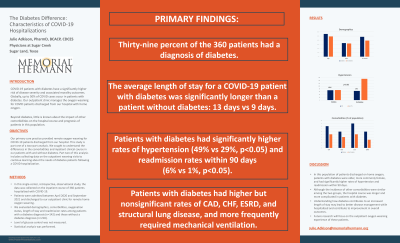
(P206) The Diabetes Difference: Characteristics of Covid Hospitalizations
Friday, August 12, 2022
12:00 PM – 1:00 PM ET
Julie Adkison, PharmD, BCACP, CDCES
Clinical Pharmacist Faculty
Memorial Hermann - Physicians at Sugar Creek
Sugar Land, Texas, United States
Primary Presenter(s)
Key Takeaways of Your Research: COVID-19 has shown a highly variable clinical presentation, ranging from asymptomatic to severe illness leading to death. Evidence indicates that, while diabetes does not increase the risk of contracting COVID-19, its presence is closely related to worse outcomes, particularly in patients with elevated A1C. Our family medicine resident physicians provided care for hospitalized patients with COVID-19. For those discharged with home oxygen, we conducted remote office visits to safely wean patients off of oxygen. The purpose of this study is to compare clinical characteristics and hospital course of this inpatient population with diabetes compared to those without diabetes.
Background/Purpose: Diabetes is a common comorbidity in patients hospitalized with COVID-19. Understanding how diabetes worsens COVID-19 outcomes can help provide better disease management and contribute to the improvement in disease outcomes. Research Hypothesis and/or Research Questions and Specific
Aims: Many factors influence disease outcome, and severe outcomes have been associated with preexisting chronic illnesses, such as hypertension and diabetes. This study compares the clinical characteristics of a COVID-19 population of 360 patients with and without diabetes discharged on home oxygen. Methods/Methodology: In this single-center, retrospective, observational study, the clinical characteristics of 360 patients hospitalized with covid-19 were collected. Patients were admitted between April 2020 and September 2021 and discharged to our outpatient clinic for home oxygen weaning. We analyzed and compared disease severity, comorbidities, oxygenation status and readmission rates among the two populations.
Results: Of the 360 patients admitted, 39% had diabetes. The average age of those with diabetes was 55 and 47% were female vs age 49 and 39% female in those without diabetes. Average BMI was 33 in the diabetes group. Patients with diabetes had nonsignificant but higher rates of CAD, CHF, ESRD, and structural lung disease, and more frequently required mechanical ventilation. Rates of diabetes patients with HTN or readmission within 90 dates met statistical significance (p < 0.05). The average length of stay for a patient with diabetes was 13 days vs 9 days in patients without diabetes. Conclusions (Impact on Diabetes Care and Education): In this population of patients discharged on home oxygen, patients with diabetes were older, more commonly female, and had significantly higher rates of hypertension and mechanical ventilation. Although rates of other comorbidities were similar, the hospital course was longer and more complicated in patients with diabetes. Further insight into these findings could provide better insight into clinical management. Source of Funding for this Research: none Authors: Julie Adkison, PharmD, BCACP, CDCES Memorial Family Medicine Residency Program, Physicians at Sugar Creek, Sugar Land, Texas.
Background/Purpose: Diabetes is a common comorbidity in patients hospitalized with COVID-19. Understanding how diabetes worsens COVID-19 outcomes can help provide better disease management and contribute to the improvement in disease outcomes. Research Hypothesis and/or Research Questions and Specific
Aims: Many factors influence disease outcome, and severe outcomes have been associated with preexisting chronic illnesses, such as hypertension and diabetes. This study compares the clinical characteristics of a COVID-19 population of 360 patients with and without diabetes discharged on home oxygen. Methods/Methodology: In this single-center, retrospective, observational study, the clinical characteristics of 360 patients hospitalized with covid-19 were collected. Patients were admitted between April 2020 and September 2021 and discharged to our outpatient clinic for home oxygen weaning. We analyzed and compared disease severity, comorbidities, oxygenation status and readmission rates among the two populations.
Results: Of the 360 patients admitted, 39% had diabetes. The average age of those with diabetes was 55 and 47% were female vs age 49 and 39% female in those without diabetes. Average BMI was 33 in the diabetes group. Patients with diabetes had nonsignificant but higher rates of CAD, CHF, ESRD, and structural lung disease, and more frequently required mechanical ventilation. Rates of diabetes patients with HTN or readmission within 90 dates met statistical significance (p < 0.05). The average length of stay for a patient with diabetes was 13 days vs 9 days in patients without diabetes. Conclusions (Impact on Diabetes Care and Education): In this population of patients discharged on home oxygen, patients with diabetes were older, more commonly female, and had significantly higher rates of hypertension and mechanical ventilation. Although rates of other comorbidities were similar, the hospital course was longer and more complicated in patients with diabetes. Further insight into these findings could provide better insight into clinical management. Source of Funding for this Research: none Authors: Julie Adkison, PharmD, BCACP, CDCES Memorial Family Medicine Residency Program, Physicians at Sugar Creek, Sugar Land, Texas.
