Back

Clinical and Self-Management Care Integration
(P102) An Inter-professional Care Team Practice Consisting of a PA, PT, and CHW
Friday, August 12, 2022
12:00 PM – 1:00 PM ET
Has Audio
.jpg)
Han-Hung Huang, PT, PhD
Associate Professor
Angelo State University
San Angelo, Texas, United States- TD
Teena Dotson, PA-C
Physician assistant-certified
La Esperanza Clinic, United States
Primary Presenter(s)
Co-Presenter(s)
Key Takeaways of Your Research: 1. Interprofessional care team practices consisting of physician assistant-certified, physical therapist and community health worker improved A1C on people with type 2 diabetes. 2. Physical therapy helps to resolve people’s challenges on body movement and minimize physical barriers to participate in physical activities or exercise. 3. The integration of professional care teams would cater to the people with diabetes individually by providing better quality care and education.
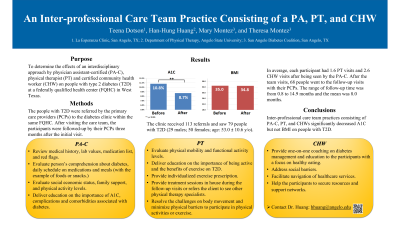
Background/Purpose: Interprofessional care team practices have been shown to be beneficial for people with type 2 diabetes (T2D). The purpose of this study is to determine the effects of an interdisciplinary approach by physician assistant-certified (PA-C), physical therapist (PT) and certified community health worker (CHW) on people with T2D at a federally qualified health center (FQHC) in West Texas. Research Hypothesis and/or Research Questions and Specific
Aims: The hypothesis is that practices with an interprofessional care team consisting of PA-C, PT, and CHWs decrease A1C and body mass index (BMI) in people with T2D. Methods/Methodology: The people with T2D were referred by PCPs within the same FQHC. The care team consisted of one PA-C, one PT, and two certified CHWs. The participants were followed-up by their PCPs three months after the initial visit. Paired sample t-test was used to compare between initial and follow-up visit. A p-value of less than 0.05 was considered statistically significant.
Results: The diabetes clinic received 113 referrals and saw 79 people with T2D (29 males; 50 females; age: 53.0 ± 10.6 y/o; A1C: 10.9 ± 1.8 %; BMI: 35.0 ± 8.9). On average, each participant had 1.6 PT visits and 2.6 CHW visits after being seen by the PA-C. After the team visits, 68 people went to the follow-up visits with their PCPs. The range of follow-up time was from 0.8 to 14.9 months and the mean was 8.0 months. The participants’ A1C significantly decreased 2.1% (p < 0.001) at their most recent follow-up visits. BMI decreased from 35.0 to 34.8 but the results were not statistically significant (p = 0.265). Conclusions (Impact on Diabetes Care and Education): Interprofessional care team practices consisting of PA-C, PT, and CHWs decreased A1C but not BMI in people with T2D. Future study is warranted to look into more clinical outcome measures (e.g., other lab values and medication doses), participant’s feedback (e.g., quality of life, physical activities, and eating habit), and cost effectiveness. Source of Funding for this Research: No outside sources of funding were used in this study. The authors have no relevant disclosures. Authors: Teena Dotson, PA-C, La Esperanza Clinic, San Angelo, TX, Han-Hung Huang, PT, PhD, Department of Physical Therapy, Angelo State University, San Angelo, TX, Mary Montez, CHW, San Angelo Diabetes Coalition, San Angelo, TX, and Theresa Montez, CHW, San Angelo Diabetes Coalition, San Angelo, TX.
Background/Purpose: Interprofessional care team practices have been shown to be beneficial for people with type 2 diabetes (T2D). The purpose of this study is to determine the effects of an interdisciplinary approach by physician assistant-certified (PA-C), physical therapist (PT) and certified community health worker (CHW) on people with T2D at a federally qualified health center (FQHC) in West Texas. Research Hypothesis and/or Research Questions and Specific
Aims: The hypothesis is that practices with an interprofessional care team consisting of PA-C, PT, and CHWs decrease A1C and body mass index (BMI) in people with T2D. Methods/Methodology: The people with T2D were referred by PCPs within the same FQHC. The care team consisted of one PA-C, one PT, and two certified CHWs. The participants were followed-up by their PCPs three months after the initial visit. Paired sample t-test was used to compare between initial and follow-up visit. A p-value of less than 0.05 was considered statistically significant.
Results: The diabetes clinic received 113 referrals and saw 79 people with T2D (29 males; 50 females; age: 53.0 ± 10.6 y/o; A1C: 10.9 ± 1.8 %; BMI: 35.0 ± 8.9). On average, each participant had 1.6 PT visits and 2.6 CHW visits after being seen by the PA-C. After the team visits, 68 people went to the follow-up visits with their PCPs. The range of follow-up time was from 0.8 to 14.9 months and the mean was 8.0 months. The participants’ A1C significantly decreased 2.1% (p < 0.001) at their most recent follow-up visits. BMI decreased from 35.0 to 34.8 but the results were not statistically significant (p = 0.265). Conclusions (Impact on Diabetes Care and Education): Interprofessional care team practices consisting of PA-C, PT, and CHWs decreased A1C but not BMI in people with T2D. Future study is warranted to look into more clinical outcome measures (e.g., other lab values and medication doses), participant’s feedback (e.g., quality of life, physical activities, and eating habit), and cost effectiveness. Source of Funding for this Research: No outside sources of funding were used in this study. The authors have no relevant disclosures. Authors: Teena Dotson, PA-C, La Esperanza Clinic, San Angelo, TX, Han-Hung Huang, PT, PhD, Department of Physical Therapy, Angelo State University, San Angelo, TX, Mary Montez, CHW, San Angelo Diabetes Coalition, San Angelo, TX, and Theresa Montez, CHW, San Angelo Diabetes Coalition, San Angelo, TX.
